Report Published October 6, 2016 · Updated October 6, 2016 · 12 minute read
Local Examples: Comprehensive Care for People with End-Stage Renal Disease
Jacqueline Garry Lampert

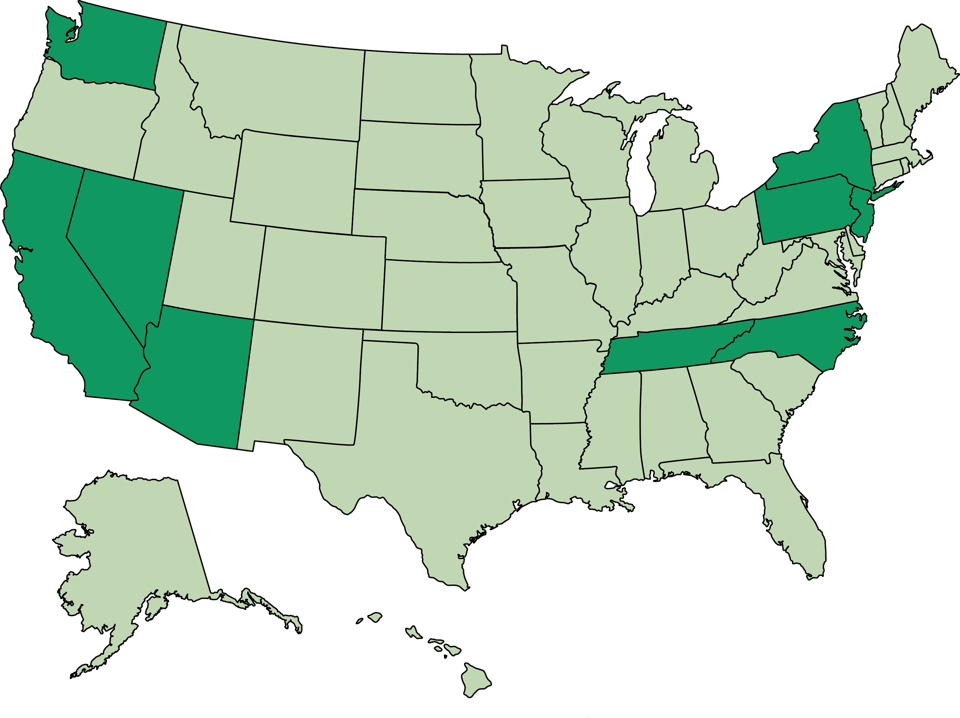
Innovative care coordination and disease management efforts to improve health outcomes and quality of life for ESRD patients are occurring through the country—providing coordinated care for people with ESRD, including personalized support for all of their health needs. Expanding these innovative models throughout Medicare could improve the lives of people living with ESRD and save Medicare money.
For example:
Nationwide
Some third party organizations offer disease management services on a contract basis with payers and providers. One example is Kidney Resource Services offered by Optum, an information and technology-enabled health services company. Optum’s Kidney Resource Services manages patients at all different stages of chronic kidney disease. Optum partners with a national Medicare Advantage plan to deliver an ESRD disease management program. The program risk-stratifies eligible individuals using claims and lab information, and utilizes registered nurse advocates to conduct outreach and care coordination that is specific to each members’ disease stage. ESRD beneficiaries enrolled in the Medicare Advantage organization’s special needs plan for dual eligible beneficiaries achieved a 25% reduction in inpatient admissions over two years. Results were positive not only for those enrolled in Optum’s disease management program, but also positive for the all of the Medicare Advantage enrollees, who saw a 24.8% reduction in inpatient admissions, a 10.3% reduction in emergency room visits, an 8.5% reduction in specialty visits, and estimated cost reduction of more than $16 million.
Arizona
The Phoenix-Tucson Integrated Kidney Care ESRD Seamless Care Organization (ESCO) is a partnership between DaVita Village Health, Banner Health, and several nephrology groups and dialysis providers in the Phoenix and Tucson area. This ESCO aims to provide high-quality care that is responsive to each patient’s needs and preferences through an integrated care management approach. Each ESCO member is assigned a specially trained nurse who works with them, their family, and the rest of their care team and has 24/7 access to a nursing team member. The nurse manager help to coordinate care received inside and outside the dialysis center and conducts patient education to help ESCO members better understand and manage their ESRD and treatment.
California
VillageHealth
Medicare Advantage Chronic Condition Special Needs Plans (C-SNPs) restrict their enrollment to individuals with certain severe or disabling chronic conditions. One of the 10 ESRD-focused C-SNPs is a partnership between VillageHealth, the renal population health management division of DaVita, Inc. and SCAN Health Plan, operating in San Bernardino and Riverside counties in California. This plan grew out of demonstration created by the Medicare Prescription Drug, Improvement, and Modernization Act of 2003, which encouraged partnerships between Medicare Advantage plans and dialysis organizations to coordinate care for ESRD beneficiaries.
VillageHealth refined its existing ESRD model of care to better serve the Medicare Advantage population, starting with a care management team consisting of nurses, social workers, dietitians, specialists, and the dialysis center staff. These care team members received specialized renal care training, and care protocols were designed to address the specific clinical needs of renal patients. VillageHealth built its own ESRD-focused technology and analytics platform, allowing for risk stratification and forecasting of patients at the highest risk for hospitalization so that care managers could engage with patients to prevent admissions. The plan’s model of care depends on collaboration with dialysis center staff and physician engagement through outcomes reporting and performance-based agreements.
Overall, the VillageHealth plan reduced non-dialysis costs compared to a similar Medicare fee-for-service sample. These cost savings were driven by population health improvements, including hospitalization and readmission rates that are 26% and 31%, respectively, lower than the national average for ESRD patients receiving dialysis. In addition, the VillageHealth plan increased fistula placement to 79% in 2013, an increase of 9 percentage points in three years. Dialysis patients require a “connection” that allows blood from an artery to flow into a vein and provide access for dialysis. An arteriovenous fistula, in which a surgeon connects an artery directly to a vein (usually in the forearm), is considered the “gold standard” given their overall performance, fewer infections that can lead to hospitalizations, durability, and allowance for increased blood flow, relative to other types of access. Finally, and perhaps most importantly, the VillageHealth plan achieved extremely high patient satisfaction, ranking among the Top 3 California SNPs for patients satisfaction between 2014-2016. VillageHealth built on the success of this plan and subsequently launched four additional ESRD C-SNPs.
CareMore
CareMore Health System, a subsidiary of Anthem, Inc. and an integrated health care company offering Medicare Advantage plans, including special needs plans, has developed a care model that centers on each individual patient and simplifies access to quality care, increases communication, and focuses on prevention and treatment. CareMore’s ESRD C-SNPs receive a four-star rating from Medicare and are available in parts of Los Angeles and Orange counties in California. CareMore aims to improve each ESRD patient’s experience and health outcomes through several initiatives, including improving health literacy about kidney disease, increasing the proportion of patients with well-planned kidney replacement therapy, addressing and improving functional status, reducing avoidable acute care utilization, and integrating and streamlining outpatient care. To achieve these goals, CareMore utilizes a care management and coordination model in which a primary care provider assumes responsibility for members’ care coordination, in close concert with a nurse practitioner-led interdisciplinary care team. Members of the interdisciplinary care team also include an internist, nephrologist, vascular surgeon and vascular access providers, dialysis center, case manager, fitness trainer, ophthalmologist, social worker, registered dietitian, podiatrist, and mental health professional.
One example of CareMore’s care redesign efforts involves hospital admissions. Before redesigning its model of care, CareMore found that half of ESRD patient admissions were the result of poor hygiene, poor diabetic control, or vascular access limits. When dialysis center staff encountered these problems, they generally referred the patient to the emergency room, which often resulted in admission. CareMore established a dedicated case manager and nurse practitioner team to receive referrals from dialysis centers. In addition, all patients enroll in a diabetes disease management program and receive monthly access line inspection and cleaning, if necessary. CareMore’s ESRD inpatient admission rate dropped to 22% below the national average, inpatient bed days fell to 73% below average, acute average length of stay was 33% lower than national average, and its readmission rate was 17% below average. Overall, its patients with chronic kidney disease have a projected 24 years on average until they have to use dialysis as opposed to less than six years under other forms of care. These results are possible because patient, provider, and payer incentives are aligned.
Fresenius Kidney Care
As more providers form accountable care organizations, dialysis providers are partnering in these alternative payment models to manage care for ACO-aligned beneficiaries with ESRD. For example, beginning in January 2013, Fresenius Kidney Care partnered Heritage California ACO. Under the arrangement, Fresenius nephrologists are participating providers in the ACO and Fresenius patients are attributed to the ACO. To facilitate care coordination, Heritage provided Fresenius access to its electronic medical record. Fresenius also has partnerships with ApolloMed ACO to provide integrated care management to ESRD beneficiaries and with Aetna to improve care quality for Medicare Advantage members with ESRD.
Nevada
Humana offers a Medicare Advantage C-SNP in Nevada, in partnership with DaVita, Inc. Like other C-SNPs, the Humana plan provides all Medicare benefits, including prescription drug coverage, organized around a model of care that is tailored to the needs of member with end-stage renal disease. DaVita’s VillageHealth nurses conduct a health risk assessment for each member to determine their current health status and needs. The nurse then works with the member and their caregiver(s) to create a plan of care based on the member’s health needs and goals. The plan of care is updated as the member’s health needs and goals change. The VillageHealth nurse is part of the interdisciplinary care team to which each member is assigned. Other primary members of this team include a nephrologist, a nurse practitioner, and the member and/or their caregiver(s), and the team may expand to include other providers as necessary given the member’s health status and goals.
New Jersey and Pennsylvania
The Philadelphia-Camden Integrated Kidney Care ESCO is an ESRD Seamless Care Organization (ESCO), part of Medicare’s Comprehensive ESRD Care model aimed at identifying, testing, and evaluating ways to improve care for Medicare beneficiaries with ESRD. In partnership with local nephrologists, dialysis providers, and the University of Pennsylvania Health System, the Philadelphia-Camden Integrated Kidney Care ESCO aims to provide integrated care to approximately 2,000 kidney disease patients in the Philadelphia area. With a team of approximately 20 clinicians and care coordinators, the ESCO staff provide patients with assistance in transitions in care, such as from the hospital to the community, medication reconciliation, and management of co-morbidities. The model of care also includes patient education and engagement, to ensure care meets each patient’s preferences and goals, and integration of clinicians more fully into the care team.
New York
The Rogosin Kidney Care Alliance is the only ESRD Seamless Care Organization sponsored by a small dialysis organization, one that has fewer than 200 dialysis facilities, participating in Medicare’s Comprehensive ESRD Care model. Rogosin serves about 400 Medicare beneficiaries in the New York City metro area with a model of care based on an interdisciplinary care team that works to provide care in line with each patient’s preferences and goals. The Rogosin Kidney Care Alliance works to coordinate care through transitions, coordinate vascular access placement and care, and coordinate provision of community-based and home health services. In addition, the ESCO provides medication management. After one year of participation, Rogosin Institute CEO Barry Smith, MD, PhD, shared that participation in this Medicare demonstration has led Rogosin to focus on things they had not paid much attention to in the past, such as depression and coordination of medication usage with non-nephrologists.
North Carolina
Providers also lead disease management and care coordination for the medically complex ESRD patient population. For example, Dialysis Clinic Inc., a large, national non-profit dialysis provider, has established a Chronic Kidney Disease Care Coordination program with the goal of preventing ESRD and the need for dialysis. The program’s goal is to reduce the number of patients who need dialysis and, if their kidney disease progresses, to educate patients on their care choices including transplant, home dialysis, center dialysis with permanent access, and medical management without dialysis. The program emphasizes transplant as the ideal ESRD therapy, both to avoid dialysis and to transition off dialysis. The program operates in 28 different settings and serves 2,800 patients at all stages of chronic kidney disease who are not on dialysis, including 18% of enrollees with stage 5 disease, or ESRD. A care coordinator begins working with patients with stage 3 chronic kidney disease to slow disease progression and stay off dialysis. Because studies show no benefit to starting dialysis before it is clinically required, the program works with patients to delay initiation of dialysis and aims to make the transition to dialysis as smooth as possible, with the first treatment ideally in and outpatient, rather than inpatient, setting.
In its Spartanburg, North Carolina, location, the Chronic Kidney Disease Care Coordination program serves 576 patients, more than are treated with dialysis at that center. The clinic is located in a nephrology office, where the care coordinator also sees patients. In this location, 29% of patients who required dialysis started at home with peritoneal dialysis—nationally this number is less than 9%. In addition, 73% of patients in the program started dialysis with a fistula and never required a catheter, compared to a national rate of only 20%. Finally, 58% of patients in the program started dialysis as an outpatient, compared to 2% of patients who started dialysis and were not in the program.
Tennessee
When Tom Bostetter was referred to Reach Kidney Care of Middle Tennessee, part of the Music City Kidney Care Alliance, he said he “never knew a thing about my kidneys.” His doctor referred him to Reach due to his decreasing kidney function, and at his first meeting with nurse practitioner Ed Dennis, Tom learned about how his lifestyle affected his kidneys and about how small changes in his diet could help him maintain kidney function. Tom now believes the changes he has made and his efforts to monitor his health aren’t difficult, he just needed someone to help him learn how. “It was the first time anyone ever opened my eyes,” Tom said.
The Music City Kidney Care Alliance is an ESRD Seamless Care Organization, part of Medicare’s Comprehensive ESRD Care model aimed at identifying, testing, and evaluating ways to improve care for Medicare beneficiaries with ESRD. The Music City Kidney Care Alliance uses a model of care that includes patient-centered education during every stage of disease to support patients in making health care decisions that reflect their preferences. Music City also offers care integration by including nephrologists, vascular surgeons, palliative and hospice care providers in the care team. It coordinates the care from all of these providers with a particular focus on care transitions. The care team relies on health information technology, including a comprehensive patient medical record, to ensure all members of the care team have accurate information about each patient. \
Washington
Two years after being diagnosed with chronic kidney failure, Patricia Smith was rushed into emergency surgery due to a spinal infection, and woke from surgery completely immobilized. As she recovered and began the long process to regain some movement, a nephrologist suggested she visit Northwest Kidney Centers’ special care unit, which could provide the kind of intensive dialysis care she needed. Here, Patricia received dialysis treatments three times a week while she worked hard in physical therapy to regain much of her lost mobility.
The special care program provides outpatient dialysis care for patients with complicated, unstable, and fragile physical, medical, or mental health statuses. Without the intensive nursing care, medication management, and care coordination provided by the special care program, most patients it serves would be hospitalized. Medicare and Medicaid do not provide additional reimbursement for the extra services provided by the special care program, which results in an unpaid cost of $2 million each year, a deficit the non-profit Northwest Kidney Center aims to make up with fundraising. But keeping these fragile patients out of the hospital reduces demands on the health care system.
