Memo Published May 1, 2025 · 5 minute read
Medicaid Cuts Would Squeeze Private Health Coverage
Darbin Wofford

As part of the partisan reconciliation process, congressional Republicans are considering $880 billion in cuts to Medicaid. While these cuts would severely impact the health and finances of low-income Americans, the consequences would reach far beyond Medicaid enrollees. Medicaid cuts would destabilize the broader health care system, ultimately driving up costs for employers and workers who rely on private insurance.
In this memo, we unpack how workers and employers are struggling with health care costs. We then examine how Medicaid cuts would squeeze health care providers and accelerate consolidation—further raising prices on care for patients with private insurance.
Workers and employers are struggling with rising health care costs.
Half of all Americans—more than 150 million people—have health insurance through the private market, primarily through the workplace. That coverage is essential, but rapidly rising costs that consistently outpace inflation mean that more than 40% of employees and their families are struggling to afford their health care.
In 2023, premiums for employer-sponsored coverage jumped by 7%, and they rose by the same amount the year before. This rapid escalation has left the average family on the hook for $6,296 in out-of-paycheck premium costs each year.
Employers are stuck fronting the remaining premium cost for each family they cover, which amounts to over $19,000 per family on average. This puts employers under significant financial strain. Employers’ premium costs ultimately affect worker pay—when companies pay more expenses, they have less to pay workers.
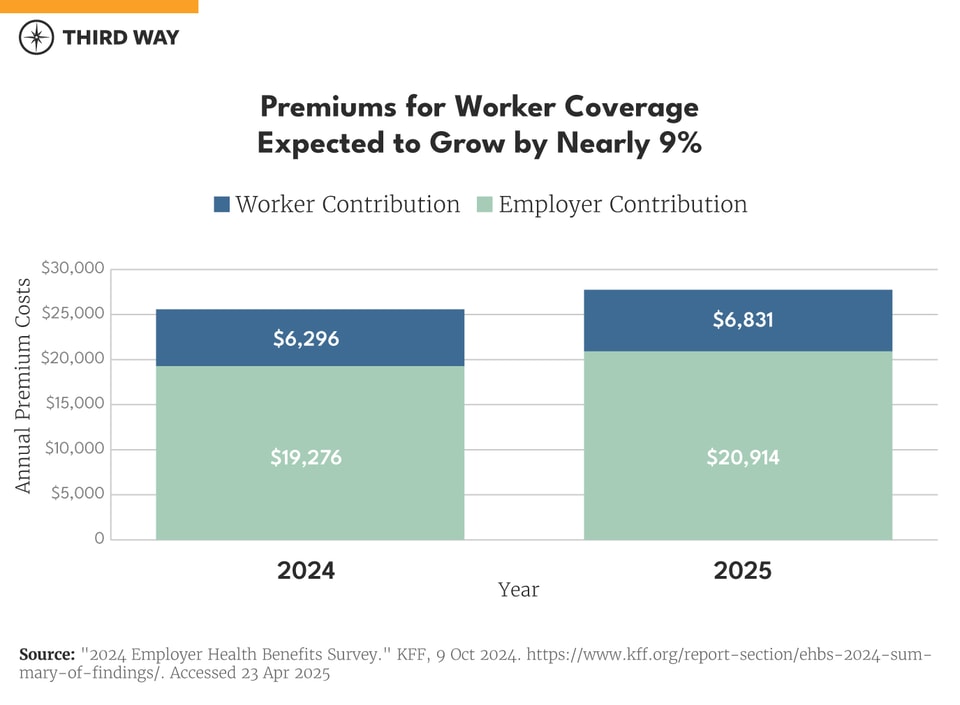
This year, premium costs are expected to rise even faster, with projections of 8-9% growth. These higher costs will be felt by businesses but also by workers through higher premiums, larger annual deductibles, and other out-of-pocket expenses. As a result, more employees with coverage will struggle to afford care. For employers, rising costs make it harder to maintain comprehensive benefits, increase wages, or reinvest in new jobs.
Medicaid cuts squeeze health care providers and accelerate consolidation.
While Medicaid is primarily known for serving low-income individuals and families, the program plays a critical role in the broader health care system.
Medicaid reimburses for health care services in hospitals, community health centers, doctors’ offices, long-term care facilities, and many others. Nearly one-in-five dollars spent on health care each year comes from Medicaid. The health care providers most vulnerable to Medicaid cuts are those serving rural and low-income communities. These providers treat higher numbers of patients with Medicaid coverage and have higher rates of uncompensated care from supplying health care to patients who are uninsured or can’t afford the out-of-pocket costs. One hundred rural hospitals have closed in recent years, and 700 more are struggling financially and at risk of shutting down.
This means that any changes to Medicaid funding can have ripple effects far beyond the program’s direct beneficiaries, impacting the financial stability of providers and the broader health care market.
Large-scale cuts to the Medicaid program would increase the number of hospitals and other providers that struggle financially. And cuts would lead to higher prices for employers when big health care systems buy up struggling hospitals. When Medicaid funding is cut, these providers are forced to absorb more uncompensated care and may have to reduce services, lay off staff, or shut down altogether. As more providers feel the financial stress of Medicaid cuts, they are more likely to consider a merger. Roughly a third of hospitals involved in merger and acquisition discussions are financially distressed.
The problem is that when a hospital is acquired by a larger system, prices increase. For example, after North Carolina-based Mission Health was acquired by HCA Healthcare, patients saw significant price hikes. Hospital mergers can lead to price increases of up to 65%. As more struggling hospitals are absorbed by larger systems, we will see higher prices and reduced competition in hospital markets. If Republicans are successful in cutting up to $880 billion from the Medicaid program, employers and patients with private insurance will see their costs rise as a result of reduced competition in hospital markets.
Hospitals less dependent on Medicaid will still raise prices—because they can.
While safety-net and rural hospitals would be hardest hit, large and more profitable health systems are typically less impacted by Medicaid cuts because they treat fewer Medicaid patients. Yet, they could seize the opportunity to raise prices for private insurers and employers anyway.
Unlike Medicaid, where hospital payment rates are set by state governments, prices in the private market are determined through negotiations between insurers or employer-sponsored plans with hospitals. In consolidated markets, these negotiations are often one-sided. Dominant hospital systems—especially those that have control over multiple facilities—can leverage their market power to demand reimbursement rates that are three or more times higher than Medicare’s. This dynamic is already straining employer-sponsored coverage, and Medicaid cuts would only worsen the problem.
If hospitals alone were to recoup their share of proposed Medicaid cuts by charging higher prices for patients, premiums and out-of-pocket costs would rise by nearly $2,000 per individual over the decade. If all health care providers were able to recoup those losses, those costs could rise by up to $6,000.1
Conclusion
Medicaid cuts may seem distant to the average worker or employer, but they will be felt in very real and direct ways. As policymakers weigh the fiscal implications of cutting Medicaid, they must also reckon with the broader consequences—especially for the millions of workers and businesses who depend on a stable, affordable private insurance market.

